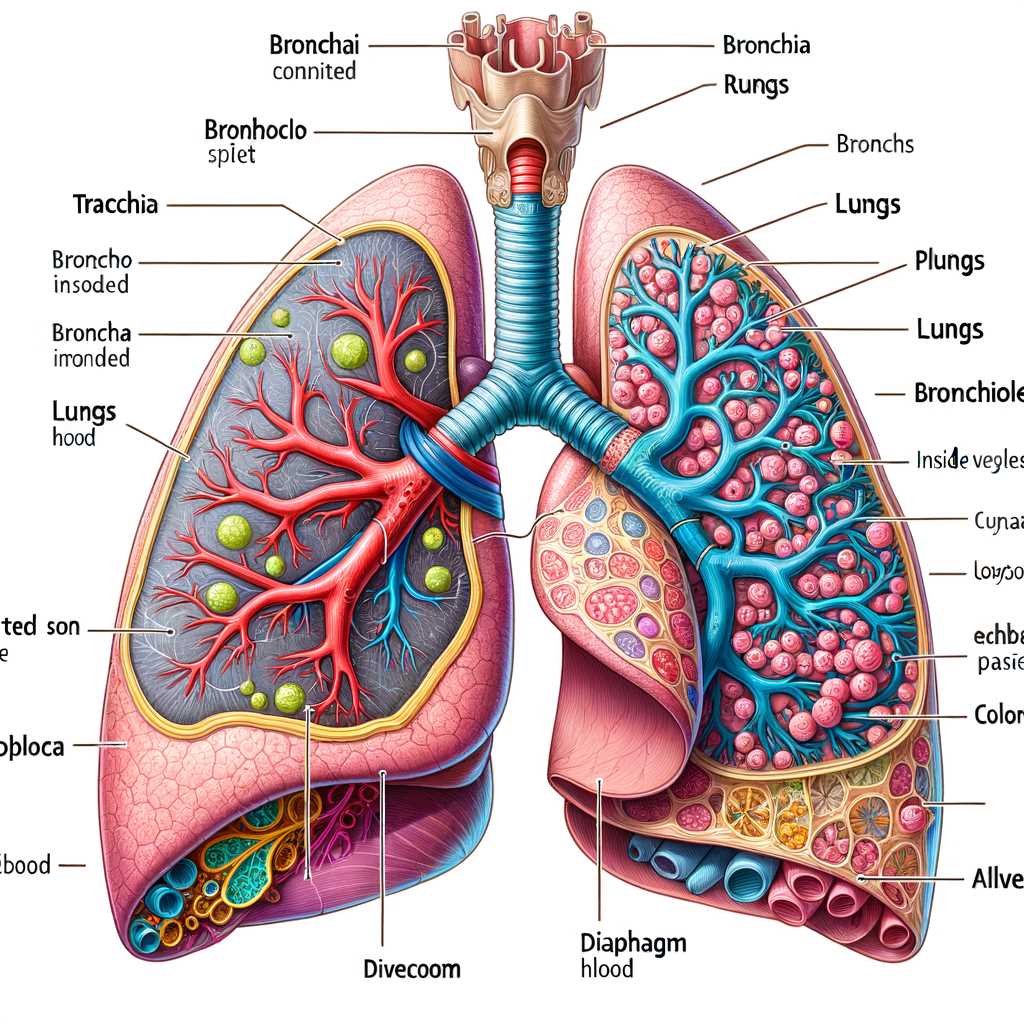
The human body’s ability to breathe is made possible by a complex network of organs working together to ensure that oxygen reaches the bloodstream while removing carbon dioxide. This intricate system plays a vital role in maintaining overall health, facilitating the exchange of gases necessary for life.
In this section, we will explore the essential components responsible for air flow, their roles in oxygen transport, and how they collaborate to support efficient gas exchange. Understanding the structure and function of these elements provides valuable insight into how breathing occurs and is regulated.
By breaking down each component’s role in the process, we can better appreciate the mechanisms behind air intake, filtering, and expelling, all of which are crucial for sustaining life.
Understanding the Structure of Human Respiration
The process of breathing is a complex interaction involving several key components, working together to sustain life. This essential function ensures the intake of oxygen and removal of carbon dioxide, maintaining the body’s balance. The human body is designed with an intricate network that allows for efficient gas exchange, supporting cellular activity and overall health.
The mechanism of breathing relies on a series of channels and organs that guide the flow of air. Each segment plays a unique role in filtering, warming, and transporting the air. This coordinated effort is what enables our bodies to function optimally, ensuring that the gases vital for survival are continuously replenished and expelled.
Central to this process is the movement of air into and out of the body, controlled by muscular contractions and relaxation. The airflow moves through a well-defined path, passing through several chambers before reaching its destination. With each inhalation, oxygen is drawn in, while every exhalation removes waste gases, completing the cycle.
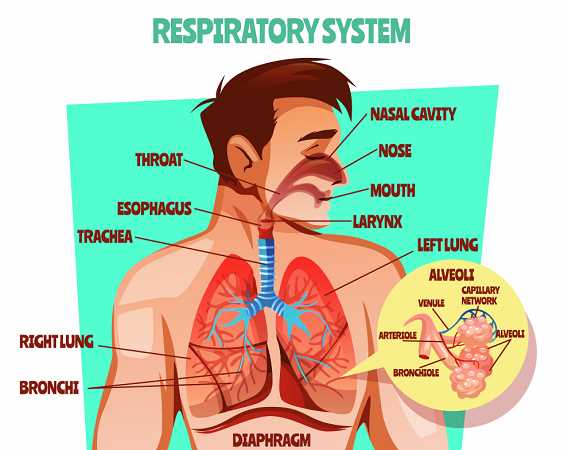
How the Nose Prepares Air for Breathing
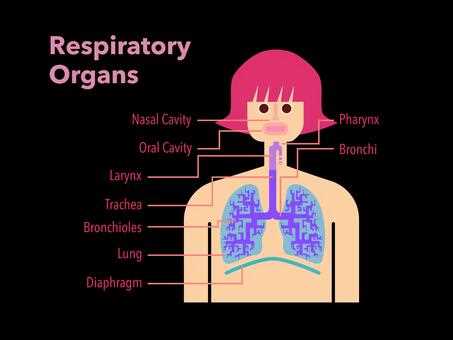
The nose plays a crucial role in ensuring that the air entering the body is clean, warm, and moist. As we breathe in, the nasal cavity begins a process that helps condition the air, making it suitable for the lungs. This natural filtration and regulation are essential for maintaining healthy oxygen intake and overall well-being.
First, the tiny hairs inside the nostrils act as a filter, capturing dust, pollen, and other small particles. This initial defense prevents harmful substances from traveling deeper. Next, the air is warmed by the blood vessels located close to the surface of the nasal passages. This step helps ensure that the temperature of the air is ideal for further travel. Lastly, moisture is added to the air by the mucous membranes, which humidify it, preventing dryness in the delicate tissues along the airways.
These processes work together seamlessly, ensuring that every breath we take is properly prepared for the body to use efficiently.
The Role of the Pharynx in Airflow

The pharynx plays a critical role in guiding air during breathing, ensuring that it passes smoothly between the nose and lungs. It serves as a passage where air is channeled, and its unique structure helps direct the flow efficiently. Understanding how this part of the airway functions can provide insight into maintaining healthy breathing patterns.
Airflow Control and Guidance
The pharynx acts as a gateway that divides incoming air into the appropriate channels. This process ensures the right direction of airflow, preventing any blockages or complications.
- Channels air from the nasal cavity toward the lower airway.
- Ensures smooth movement by keeping the passage clear of obstructions.
- Coordinates with other structures to optimize air movement.
Protection and Coordination
This airway segment not only guides air but also plays a protective role. By ensuring proper closure when needed, it helps prevent food and other substances from entering the lungs.
- Closes during swallowing to protect the airway.
- Coordinates with the larynx and esophagus to maintain proper function.
- Helps filter and warm the air before it reaches the lungs.
How the Larynx Controls Air Passage
The larynx plays a key role in managing the flow of air to and from the lungs. Its structure allows it to act as a gateway, adjusting the airflow as needed. This ensures smooth inhalation and exhalation while also protecting the airways from potential hazards.
Role of the Vocal Cords
Within the larynx, the vocal cords are pivotal in controlling the passage of air. They tighten or loosen based on the body’s needs, creating narrow or wider openings. This mechanism not only regulates breathing but also allows for sound production during speech.
Epiglottis as a Protective Barrier
The epiglottis, another essential component, acts as a shield by closing the entryway to the trachea during swallowing. This prevents food and liquid from entering the airway, ensuring that airflow remains uninterrupted when breathing resumes.
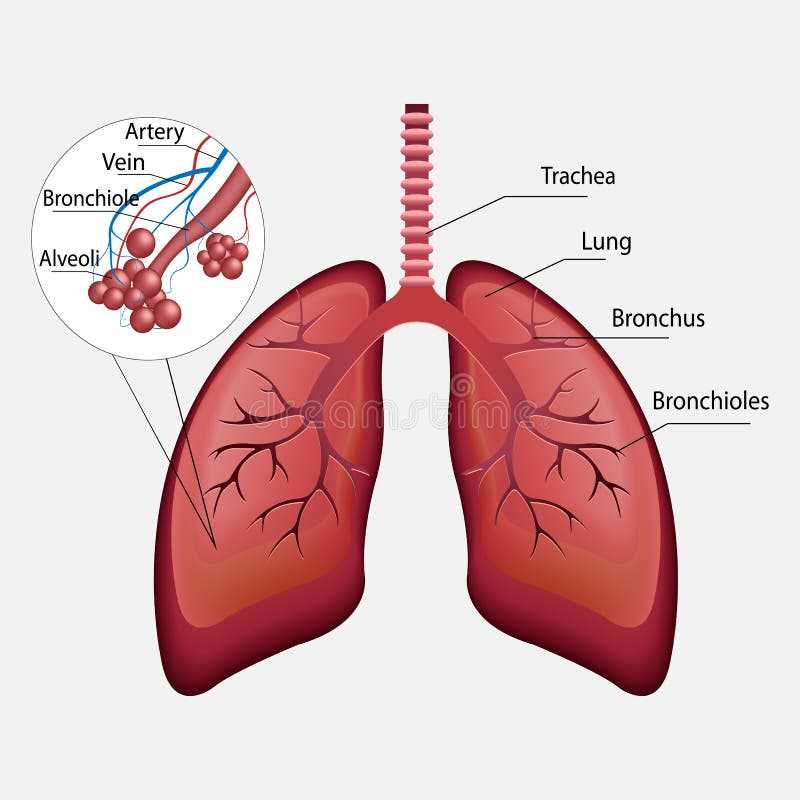
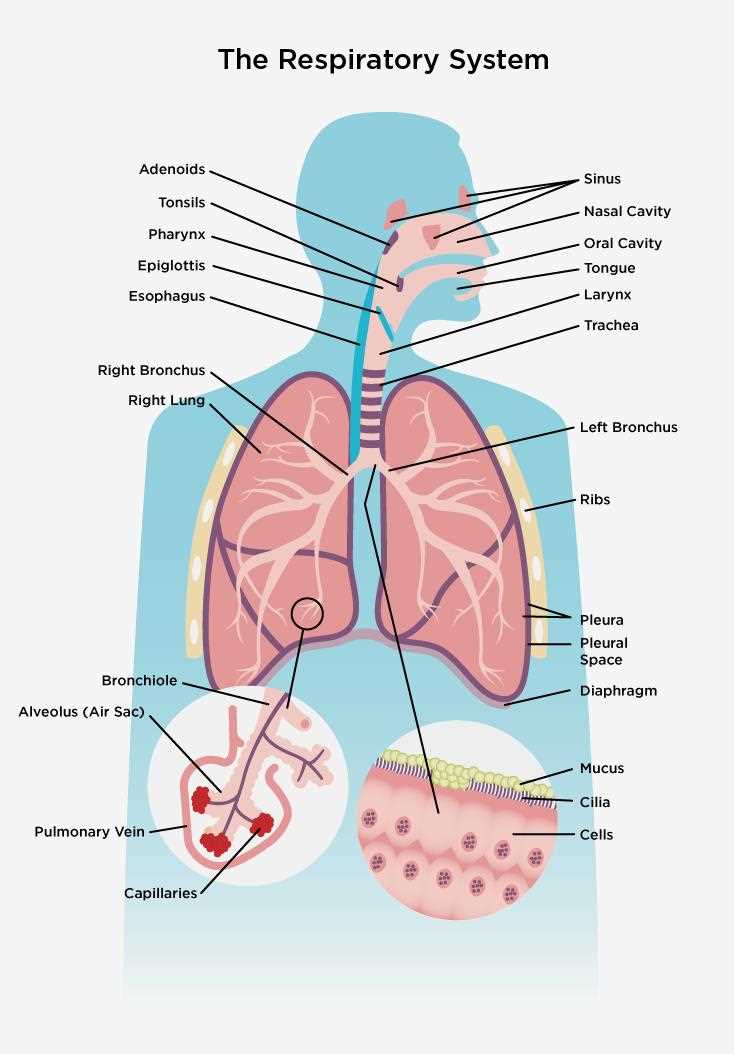
Functions of the Trachea in the Respiratory Process
The trachea plays a critical role in ensuring that air reaches the lungs safely and efficiently. It acts as a vital conduit, providing a clear path for airflow. This tubular structure is designed to maintain stability and protect the passage of air, while simultaneously responding to environmental conditions.
One of the key functions of the trachea is to filter, warm, and moisten the air before it reaches the lungs. The inner lining of the trachea is equipped with specialized cells that trap foreign particles, preventing them from entering deeper into the airways. Additionally, the trachea contains cartilage rings that keep it open, allowing for uninterrupted airflow.
Below is a breakdown of the main functional aspects of the trachea:
| Function | Description | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Air Conduction | Ensures that air flows freely to and from the lungs. | ||||||||||||||||||||||
| Air Filtration | Traps dust, pollen, and other particles using mucus and cilia. | ||||||||||||||||||||||
| Air Humidification | Moistens incoming air, protecting delicate lung tissues. |
| Feature | Description |
|---|---|
| Structure | Small, tubular branches from the bronchi |
| Muscle Type | Smooth muscle for regulation of airflow |
| Function | Direct air to the alveoli for gas exchange |
| Branching | Continues to divide into smaller passages called terminal bronchioles |
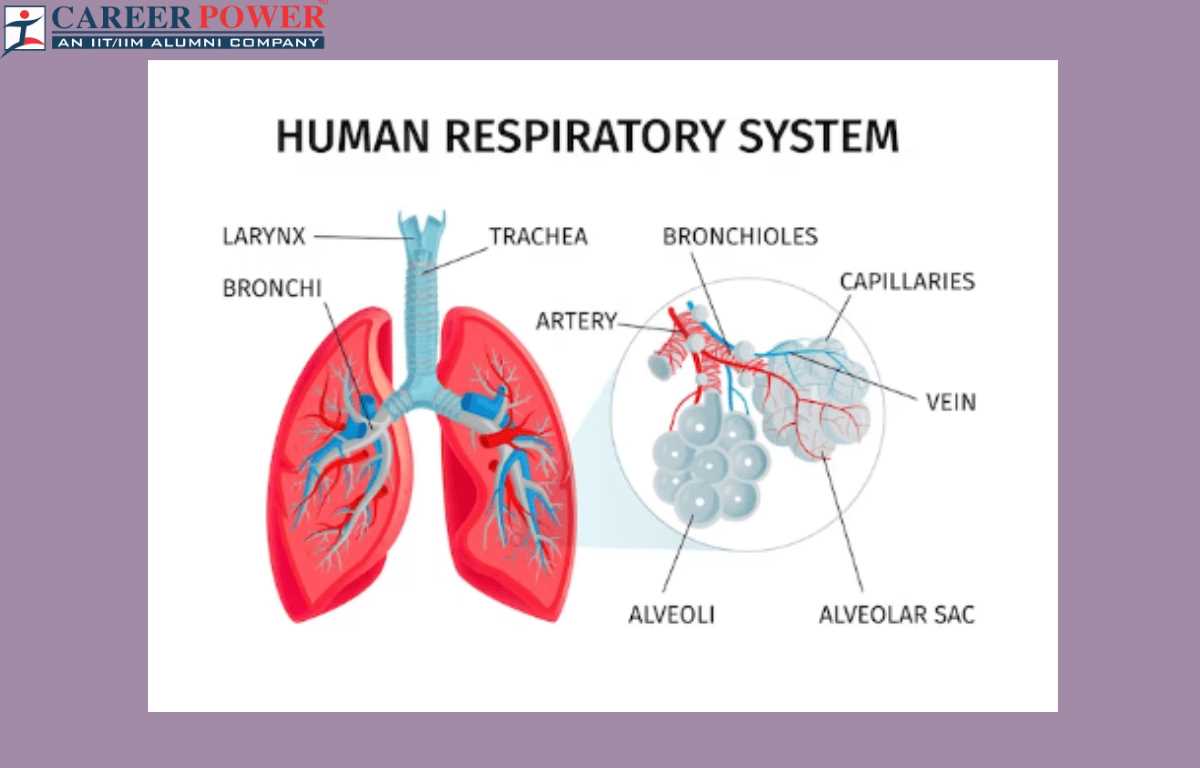
The terminal bronchioles represent the final segment of the conducting airways, transitioning into the respiratory bronchioles, where the alveoli begin to emerge. This transition marks a crucial shift from purely air conduction to areas where oxygen and carbon dioxide can be exchanged, highlighting the essential nature of bronchioles in overall pulmonary function.
How the Alveoli Facilitate Gas Exchange
The alveoli play a crucial role in the exchange of gases within the body, acting as the primary site where oxygen is absorbed and carbon dioxide is expelled. These tiny, balloon-like structures are designed to maximize the surface area available for this vital process, ensuring that efficient transfer of gases occurs between the air and the bloodstream.
Each alveolus is surrounded by a network of capillaries, which are small blood vessels that facilitate the movement of oxygen and carbon dioxide. When air enters the lungs, it fills these alveoli, allowing oxygen to diffuse through their thin walls into the blood. At the same time, carbon dioxide, a waste product produced by cellular metabolism, moves from the blood into the alveoli to be exhaled. This exchange occurs due to differences in concentration gradients, with gases moving from areas of higher concentration to areas of lower concentration.
The structure of the alveoli is specifically adapted to enhance this gas exchange process. Their walls are extremely thin, composed of a single layer of epithelial cells, which minimizes the distance gases must travel. Additionally, the presence of a surfactant reduces surface tension, preventing the alveoli from collapsing and ensuring they remain open for efficient gas exchange.
In summary, the alveoli are essential components that enable the body to obtain oxygen and eliminate carbon dioxide effectively. Their unique structure and functional design optimize the gas exchange process, making them vital for maintaining overall health and supporting cellular function.
Understanding the Diaphragm’s Role in Breathing
The diaphragm is a crucial element in the process of inhalation and exhalation. This dome-shaped muscle acts as a barrier between the thoracic cavity and the abdominal cavity, playing a significant role in the mechanics of ventilation. When it contracts, it flattens and expands the thoracic cavity, allowing air to flow into the lungs. Conversely, during relaxation, it returns to its original position, facilitating the expulsion of air.
This muscle not only supports breathing but also contributes to various bodily functions. It aids in regulating intra-abdominal pressure, which is essential for activities such as digestion and childbirth. Moreover, the diaphragm assists in enhancing circulation by promoting venous return to the heart, thus supporting overall cardiovascular health.
Understanding the function of the diaphragm provides insights into maintaining optimal respiratory efficiency. Various breathing techniques emphasize its importance, promoting deeper and more effective breaths. Recognizing how this muscle operates can lead to improved respiratory habits, benefiting both physical performance and relaxation.
Intercostal Muscles and Their Role in Respiration
The intercostal muscles play a vital role in the process of breathing by facilitating the expansion and contraction of the thoracic cavity. These muscles are situated between the ribs and are essential for the mechanics of inhalation and exhalation. Their coordinated actions ensure that air flows in and out of the lungs effectively, contributing significantly to overall pulmonary function.
Types of Intercostal Muscles
There are two primary types of intercostal muscles: external and internal. The external intercostals are responsible for elevating the ribs during inhalation, which increases the volume of the thoracic cavity and allows air to enter the lungs. In contrast, the internal intercostals assist in forced exhalation by depressing the ribs and decreasing the volume of the thoracic cavity, promoting the expulsion of air.
Importance in Breathing Mechanics
The intercostal muscles work in concert with the diaphragm, the main muscle of respiration. During deep or rapid breathing, these muscles become more active, allowing for greater air intake. Proper functioning of the intercostal muscles is crucial, as any impairment can lead to difficulty in breathing, reduced oxygen supply, and increased effort during respiration. Understanding their mechanics highlights the complexity of the breathing process and the importance of these muscles in maintaining efficient pulmonary ventilation.
The Importance of Pleura in Lung Function
The pleura plays a vital role in facilitating optimal lung performance and maintaining overall pulmonary health. This thin, double-layered membrane surrounds each lung, providing essential protection and support during the breathing process. Its unique structure contributes significantly to the efficiency and functionality of the lungs.
Key functions of the pleura include:
- Reduction of Friction: The pleural layers produce pleural fluid, which acts as a lubricant. This fluid allows the lungs to expand and contract smoothly against the thoracic wall, minimizing friction during inhalation and exhalation.
- Pressure Regulation: The pleura helps maintain a negative pressure in the pleural cavity, which is crucial for lung inflation. This pressure differential allows the lungs to expand effectively, ensuring adequate gas exchange.
- Protection: The pleura serves as a barrier against infections and external agents. It provides a protective covering, reducing the risk of injury and inflammation that could impair lung function.
Overall, the pleura is essential for efficient respiratory mechanics. Its ability to reduce friction, regulate pressure, and protect lung tissues ensures that the lungs can perform their vital functions effectively.
How Oxygen Travels Through the Bloodstream
The journey of oxygen through the circulatory network is vital for sustaining life. It begins as air is inhaled, filling the lungs and facilitating the transfer of this essential gas into the bloodstream. This process ensures that every cell in the body receives the necessary fuel for energy production and metabolic activities.
Once inside the lungs, oxygen molecules bind to hemoglobin, a protein found in red blood cells. This binding is crucial, as hemoglobin acts as a transport vehicle, carrying oxygen throughout the body. The red blood cells, now rich in oxygen, flow through blood vessels, delivering this precious resource to tissues and organs.
| Stage | Description |
|---|---|
| Inhalation | Air enters the lungs, allowing oxygen to diffuse into the bloodstream. |
| Binding | Oxygen binds to hemoglobin in red blood cells, forming oxyhemoglobin. |
| Circulation | Oxygen-rich blood travels through arteries to various parts of the body. |
| Release | Oxygen is released from hemoglobin into body tissues, supporting cellular functions. |
| Return | Oxygen-depleted blood returns to the lungs for re-oxygenation. |
This continuous cycle of oxygen transport is fundamental for maintaining health and vitality. Without this intricate mechanism, the body would struggle to meet its energy demands, highlighting the importance of efficient gas exchange and circulation.
Link Between the Respiratory and Circulatory Systems
The intricate relationship between the breathing and blood circulation networks is vital for sustaining life. These two vital mechanisms work in tandem to ensure that the body receives the necessary oxygen while eliminating carbon dioxide efficiently. Understanding how these two systems interconnect reveals the complexity of physiological processes essential for overall health.
When air enters the lungs, oxygen is extracted and transported into the bloodstream. This exchange takes place in tiny air sacs known as alveoli. Here’s a breakdown of the process:
- Inhalation: Air flows into the lungs, filling the alveoli with oxygen-rich air.
- Gas Exchange: Oxygen diffuses through the alveolar walls into the capillaries, where it binds to hemoglobin in red blood cells.
- Transportation: The oxygenated blood is pumped from the lungs to the heart, which then distributes it throughout the body.
Simultaneously, carbon dioxide, a waste product produced by cells during metabolism, is transported back to the lungs. This occurs as follows:
- Carbon dioxide diffuses from the tissues into the bloodstream.
- It travels back to the lungs, where it is expelled during exhalation.
This continuous cycle not only ensures that every cell receives the oxygen it requires but also maintains acid-base balance in the body, contributing to homeostasis. Any disruption in this interplay can lead to significant health issues, emphasizing the importance of both mechanisms working harmoniously.